We have been writing about
coronavirus for a while. We have
mentioned that we had 120 patients treated with steroids -cero deaths at the
end of June; we have around 400 now. Our
article was written before the appearance of articles related to dexamethasone and
coronavirus. Dexamethasone was
prohibited as a medication for COVID 19 by the WHO and the CDC at the begining of the pandemic, it was accepted
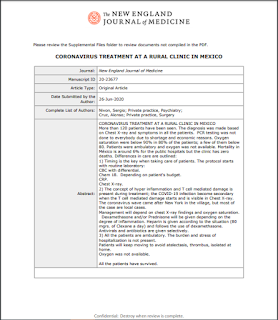
for the very ill later. The photo screenshot
of the abstract sent to the NEJM is below.
The article was not reviewed by the journal. We did not use antivirals
because they were not specifics, assuming what we know about the use of dexamethasone
in HIV positive patients. This wonder
drug rescued Trump from dropping oxygen saturations episodes. It was not Remdesivir the wonderful drug. Until he got dexamethasone, Trump felt better
and could breathe better. This very
cheap drug can save millions of lives related to coronavirus and not a vaccine or
the antivirals. The problem is that dexamethasone
is not business (money). It was
advertised for the severely ill but we can use when we see the shortness of
breath and desaturation. C-reactive
protein could be as low as 2.
8 juin
2020
Triathlon and Coronavirus Treatment in Oaxaca II
We mentioned the reason why we post
this subject here: we do not have other place to post
it. Mexico is the third country in the Americas regarding the number
of contagious people and respective deaths. We are at the peak of
the epidemic at the present time. We come from this small city in
Mexico and we speak about a village near Oaxaca where we follow up patients
with covid 19. Our friend is the one on the frontline, we just
support him. The price for each treatment is $5,000.00 pesos ($220
dollars), so people can afford it. $25.00 dollars for the initial consultation
and the rest is for medications. Close to 100 patients with covid 19
and zero deaths.
We can start talking why patients are
not dying as it is the case in Mexico where mortality is around
6%. Two things are present:
1) Excellent service and
follow up. Timing is the key when taking care of patients.
1.1) The protocol
starts with routine laboratory:
CBC with differential.
Chem 18.
CRP.
Chest X-ray.
1.2) Management will
depend on findings. Antivirals and antibiotics are given routinely. Prednisone
will be given depending on the degree of inflammation. Prednisone
because is the cheapest, it exists in any pharmacy stock, and it is well known
to us (starting with 50 mgrs). Heparin is given according to the
situation (80 mgrs. of Clexane a day).
2) The burden and
stress of hospitalization is not present.
2.1) Patients will
keep moving to avoid atelectasis, thrombus and interestingly they have better
ventilation.
2.2) Oxygen was not given because it
was not available but we have learned that even when they have O2 saturation in
the low 80, they can still move and they have a good outcome from what we know
(no one has died).
Taking care of patients is similar to taking care of
athletes. Attention to details is important. Athletes and
patients should know that they are getting the best care
available. They have to believe in what we are
doing. Science as Albert Einstein puts it and it should be present:
“Science is the refinement of every day thinking; common sense thinking.”
I let you enjoyed the lake where we train in Oaxaca.
We follow
our own protocol:
21 avr.
2020
Triathlon and Team
Oaxaca Coronavirus Guidelines
We started learning since the
beginning of the pandemic about the virus, to face the situation. We
have learned the following:
1) The virus is
transmitted via aerosol in addition to saliva
drops. Why? We have the story about the chorus rehearsing
and apparently keeping the distance between two people. They said:
“No one sneezed or coughed.” One-day rehearsal, 60 people
practicing, 45 sick, two deaths. https://edition.cnn.com/2020/04/01/us/washington-choir-practice-coronavirus-deaths/index.html This is more
anecdotal, if you wish, but we have other sources of information.
We have the studies mentioned in the
New England Journal of Medicine:
Surgical
Masks Provide Source Control of Respiratory Viruses
Richard T. Ellison III, MD reviewing Leung
NHL et al. Nat Med 2020 Apr 2 Bae S et al. Ann Intern
Med 2020 Apr 6
Surgical face masks were
found to reduce presence of influenza and coronavirus RNA in respiratory droplets
and aerosols from infected individuals.
The CDC has just
recommended that the general U.S. population begin wearing cloth face coverings
to decrease the community-based transmission of the SARS-CoV-2 virus. Two new
studies provide some support for the CDC guidelines.
In the first,
researchers at a Hong Kong hospital obtained nasal and throat swabs and
respiratory droplet and aerosol samples from 246 individuals with presumed
symptomatic acute respiratory viral infection seen year-round between March
2013 and May 2016. During a 30-minute collection of exhaled breaths when
patients were breathing and coughing normally, 124 individuals were wearing a
face mask and 122 were not; 49 provided second 30-minute samples of the
alternate type.
By reverse transcriptase
polymerase chain reaction (RT-PCR) there were 54 individuals with rhinovirus
infection, 43 with influenza infection, and 17 with human seasonal coronavirus
infection. For all three viruses, the viral load was higher in nasal than in
oral secretions, and all three viruses were detectable in both respiratory
droplet (particles >5 μm) and aerosol (particles <5 μm) fractions of the
exhaled breath. Masks led to a notable reduction in the number of
RT-PCR–positive respiratory droplet and aerosol samples for patients with either
coronavirus (in respiratory droplets, from 30% to 0%; aerosols, 40% to 0%) or
influenza infection (respiratory droplets, 26% to 4%; aerosols, 35% to 22%);
there was no meaningful reduction seen with rhinovirus infections. Influenza
virus was able to be grown from 4 of 5 studied RT-PCR–positive aerosol samples
from individuals not wearing masks.
The second study, by Bae
and colleagues, recruited 4 patients with SARS-CoV-2 infection to cough five
times onto petri dishes containing viral transport media approximately 20 cm
from their face while wearing either no mask, a surgical face mask, or a
two-ply cotton mask. The median nasopharyngeal viral load was 5.66 log
copies/mL, and the cough samples found viral loads of 1.4 to 3.5 logs/mL
whether or not a mask was present for three of the four patients. Swabs of the
outer surfaces of both types of masks were positive for all four patients.
COMMENT
The work by Leung raises
the theoretical concern of viral transmission through aerosols as well as
respiratory droplets although, as the authors note, there was no attempt to
grow either coronavirus or rhinovirus from the RT-PCR respiratory samples to confirm
the presence of viable virus. Still, this novel study provides strong evidence
that the use of surgical masks can provide source control for both human
coronavirus and influenza virus infections when individuals are sitting for 30
minutes. In contrast, the very small study by Bae shows that neither surgical
nor cotton face masks will prevent the spread of virus from a coughing
individual — at least at a distance of only 20 cm. While both studies have
clear limitations, together they suggest that the use of a surgical face mask
can provide some source control in individuals infected with coronavirus or
influenza, although the efficacy is likely diminished in coughing individuals
(and we can't extrapolate the findings to other types of masks). Still, in my
mind these limited data do support the broad use of face masks until this
pandemic is brought under control.
2) The German expert
who instituted the program in Germany challenged the notion that the virus is
primarily acquired touching infected material. The assumption was
that the coronavirus is transmitted via air and not so much by contact.
Researchers have so far come to
different conclusions on how long the virus can survive on surfaces. But now a
team of scientists in Germany are trying to find answers.
"So far, no transmission of the
virus in supermarkets, restaurants or hairdressers has been proven,"
explained Bonn virologist Hendrik Streeck on the ZDF Markus Lanz talk show.
Instead, the major outbreaks have
been the result of close get-togethers over a longer period of time, he said.
That's demonstrated in, for example,
outbreaks that have stemmed from après-ski parties in Ischgl, at football
matches in Bergamo or at carnival celebrations in the municipality of Gangelt
in the Heinsberg district of North Rhine-Westphalia.
3) The lakes, ocean
are not infected to the degree of being a source of infection. The
problem is that we still get aerosol from infected people because those places
are crowded most of the time. The infection is not in the water.
https://www.unwater.org/coronavirus-global-health-emergency/
Coronaviruses (CoV) are a large family
of viruses that cause illness ranging from the common cold to more severe
diseases. According to WHO, while persistence in drinking-water is possible,
there is no current evidence that coronaviruses are present in surface or
groundwater sources or transmitted through contaminated drinking-water.
The spread of the virus is closely related to water and
sanitation.Cleaning hands can reduce the transmission and help people stay
healthy but today billions of people lack safe water, sanitation and
handwashing and funding is inadequate.
Based on the above:
1) Keep your distance,
two meters from other human being.
2) Wear a face mask
according to what you do. Driving a car with other triathletes, wear
a N95 mask; use a surgical mask when riding or running with other mates,
keeping most of the time the two meters of separation.
3) Swim in an empty
swimming pool, one member per lane or in a lake (keeping distance).
4) Wash your hand as
frequently as you can or use gel (alcohol above 60%).
5) Avoid public places
or wear your N95 if you need to be in a close room, even if you keep the two
meters distance (remember the chorus rehearsal).
6) Train with
responsible people that is concerned about his/her health and the health of
others. This is the moment to define your friends.
7) This should be in
place until we obtain the vaccine or we get 70% infected people. I
hope the vaccine comes first.